When couples struggle to conceive naturally, assisted reproductive technologies like IVF (In Vitro Fertilization) and ICSI (Intracytoplasmic Sperm Injection) offer a beacon of hope. However, these two procedures are not interchangeable for every patient. Infertility specialist carefully evaluate multiple factors before deciding which method is best.
What is IVF?
IVF involves collecting eggs and sperm, fertilizing them in a lab dish, and then transferring the resulting embryo(s) into the uterus. In standard IVF, the egg and thousands of sperm are placed together in a culture dish. One of the sperm naturally fertilizes the egg.
What is ICSI?
ICSI is a specialized form of IVF where a single healthy sperm is directly injected into the egg using a fine needle under a microscope. This method bypasses natural fertilization steps, making it ideal for specific male infertility issues.
Step-by-Step Decision Process by Fertility Specialists
Infertility specialists follow a detailed approach to decide between IVF and ICSI. Here’s how they do it:
1. Semen Analysis
This is often the first and most crucial test.
Low Sperm Count (Oligospermia): If the sperm count is below normal, there may not be enough sperm to fertilize the egg naturally, even in a lab setting. ICSI is usually recommended.
Poor Motility (Asthenozoospermia): When sperm can’t swim properly, reaching and penetrating the egg becomes difficult. ICSI overcomes this by injecting the sperm directly into the egg.
Abnormal Morphology (Teratozoospermia): If the shape of the sperm is abnormal, fertilization may fail in standard IVF, making ICSI a better option.
Azoospermia: If no sperm is found in the ejaculate, but viable sperm are retrieved surgically, ICSI is used to fertilize the egg with these limited sperm cells.
2. Previous IVF Failures
If a couple has undergone IVF and experienced failed fertilization, ICSI may be used in subsequent cycles. Poor fertilization could mean the sperm can’t penetrate the egg’s outer layer—a problem that ICSI can bypass.
3. Sperm Retrieval Methods
In some male infertility cases, sperm must be collected surgically through procedures like:
TESA (Testicular Sperm Aspiration)
PESA (Percutaneous Epididymal Sperm Aspiration)
These samples often contain fewer or weaker sperm, making ICSI the preferred choice over conventional IVF.
4. Female Egg Factors
While ICSI is typically used for male infertility, in some cases, it may be selected due to egg-related issues:
Thick Zona Pellucida: The outer layer of the egg may be too thick for sperm to penetrate naturally.
Post-thaw Eggs: Frozen eggs may have a hardened outer layer, making natural fertilization harder. ICSI is preferred in such cases.
5. Use of Donor Sperm or Eggs
When using donor sperm that meets normal parameters, IVF may be sufficient. However, if there is any question about the quality, ICSI may be advised.
Similarly, when using donor eggs, particularly those that have been frozen, specialists may lean toward ICSI for higher fertilization rates.
6. Genetic Concerns
If there is a risk of genetic disorders, couples might undergo PGT (Preimplantation Genetic Testing). Since PGT requires fertilized embryos, and ICSI minimizes the risk of contamination with external sperm, it is the preferred method for such cases.
7. Unexplained Infertility
In couples where no clear cause of infertility is found, and standard IVF has not resulted in successful fertilization, ICSI may be used as a precaution to increase chances of fertilization.
8. Financial and Ethical Considerations
In some clinics or countries, cost is also a deciding factor. ICSI is generally more expensive than IVF due to the specialized equipment and labor involved. If there is no medical need for ICSI, specialists may recommend IVF first to manage cost without compromising success.
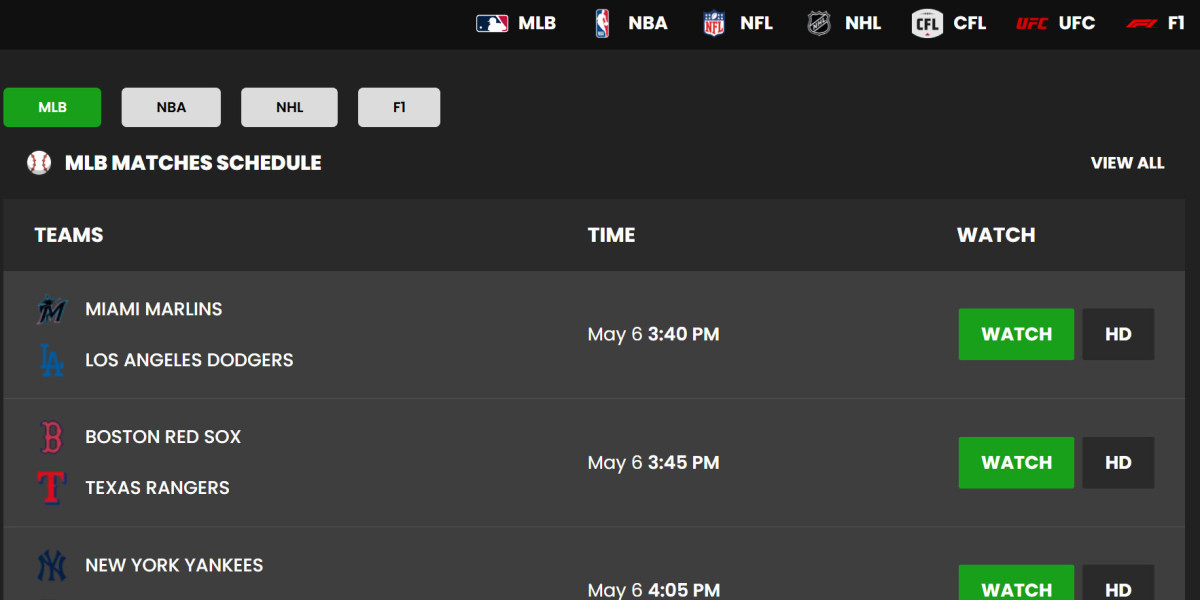
IVF vs. ICSI – At a Glance
| Feature | IVF | ICSI |
|---|---|---|
| Sperm Requirement | Normal sperm count & motility | Very few or low-quality sperm needed |
| Egg Fertilization Method | Natural fertilization in lab dish | Direct sperm injection into egg |
| Common Use | Female infertility, unexplained | Male infertility, past IVF failure |
| Cost | Lower | Slightly higher |
| Success in Male Factor | Moderate | High |
What Do Global Guidelines Say?
Organizations like ASRM (American Society for Reproductive Medicine) and ESHRE (European Society of Human Reproduction and Embryology) recommend reserving ICSI for cases with:
Male factor infertility
Fertilization failure in prior IVF cycles
Use of frozen or surgically retrieved sperm
They advise against routine ICSI use when there’s no clear benefit, as studies show it doesn’t increase pregnancy rates in non-male factor cases.
Conclusion:
The decision between IVF in Lahore and ICSI is not one-size-fits-all. Fertility specialists evaluate every couple individually looking at sperm health, egg quality, past IVF outcomes, and overall reproductive health. ICSI is a breakthrough technology that has allowed many men with severe infertility to become biological fathers. Yet, for couples without male infertility, standard IVF often works just as well.
At centers like the Australian Concept Infertility Medical Center, fertility decisions are guided by a thorough diagnosis and tailored treatment plans. The right method—IVF or ICSI—depends on science, experience, and your unique reproductive journey.